Diverticulitis and Diverticular disease
What is Diverticulitis and Diverticular disease?
Diverticulum is a small out-pouching from the wall of the gut.
Diverticulae mean mores than one diverticulum. They can develop on any part of the gut but most often in the large bowel (colon) on the left side. They tend to be multiple and this is called diverticulosis. If they cause symptoms then this is known as diverticular disease and if they become infected or inflamed this is called diverticulitis. See the diagram below from Guts UK.
Diverticulae are common, particularly as we get older. Approximately half the population aged over 50 have diverticulae in their colon and this rises to 70% by 80 years of age. Men and women are equally affected.
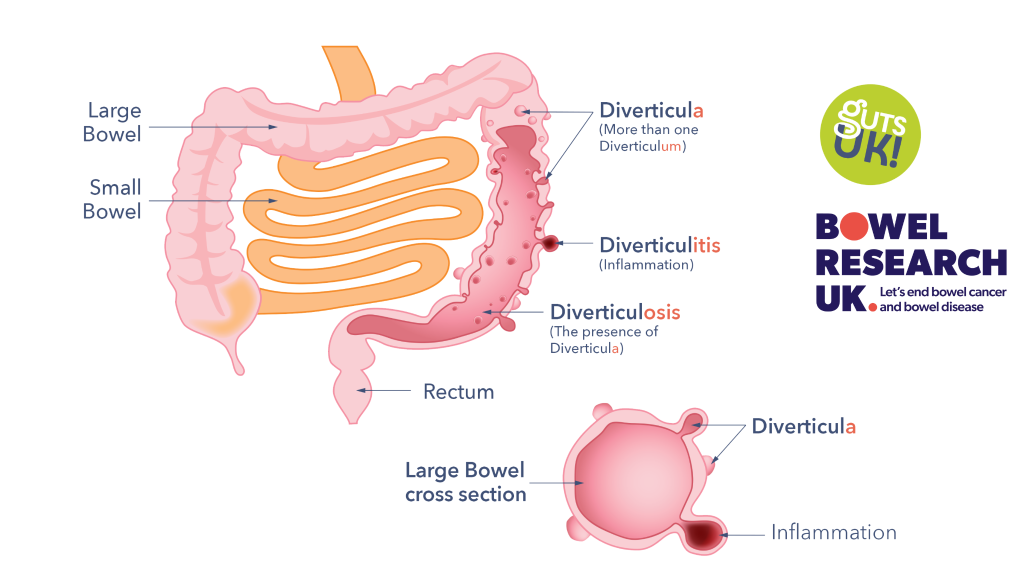
Diagram from Guts UK
Symptoms of diverticulitis and diverticular disease
Most people never know they have diverticulae and have no symptoms. Some people may get bloating and/or crampy pain in the abdomen which is eased by going to the toilet.
However in some people they may become more problematic. If stools get trapped in them, bacteria will then multiply and cause infection. The symptoms include pain in the abdomen (usually left sided), fever, constipation or diarrhoea and/or blood mixed in your stool. If the infection is severe, a collection of infection (abscess) may form.
How is diverticulitis and diverticular disease diagnosed?
How is diverticulitis and diverticular disease treated?
Outcomes and further sources of support
What to ask your Doctor?
These are some useful questions you can ask your doctor:
- Has my colonoscopy/CT scan ruled out any other conditions?
- Are there any issues of potential concern in my large bowel?
- Would you refer me to a dietitian for further help with my diet?
- What monitoring or follow up will I be offered?
- When will antibiotics be considered when treating my diverticulitis and when should I seek further advice?
What can I do?
Contact your GP and use the information on our website to inform you. You can also visit the NHS Website.
Please note we are not able to offer any medical advice – please contact the NHS for such enquiries on the website above.
What is Bowel Research UK doing?
Bowel Research UK and Guts UK are collaborating on a Priority Setting Partnership for diverticular disease. We’re excited to work with Guts UK and interested patients, carers and healthcare professionals on this brand new project.
What is a Priority Setting Partnership?
A Priority Setting Partnership or PSP is a project that aims to discover the top ten research priorities for a health condition. It brings together patients, carers, researchers, and healthcare professionals to find out what really matters in a particular area. We are working with the James Lind Alliance to set up this PSP, which will identify and prioritise unanswered questions around diverticular disease. A PSP is just the beginning of research, as once the top ten priorities are identified, other researchers can use this to decide what to research in order to provide diverticular disease patients with the help they need the most.